Making Treatment Decisions in the ICU
Patients in the ICU usually can’t communicate – Dr. Heyland explains the role of the Subsitute Decision Maker and how to use My ICU Guide to think about the care that would be best for your loved one.
*Click CC in the play bar or C on your keyboard for subtitles/closed captions
- Possible Treatment Decisions
- Who represents the patient if they can’t speak for themselves?
- What is your role as Substitute Decision Maker?
- What do you think would be most important to your family member?
- What is the doctor’s role?
- What you can expect from your Doctor?
- Do I have to make decisions alone?
- If the Patient Does Not Survive
Many patients in the ICU are unable to make their own medical decisions.
In these situations, knowing if they have already communicated their wishes or written them down can be helpful in making decisions about the treatments your family may receive. The medical team will want to review with you the overall goals of care. For some ICU patients, treatment with life-sustaining therapies is time-limited.’ One of the most important decisions that may arise is whether to continue using invasive technologies to prolong life alongside medical management and symptom control, or to focus only on medical management and symptom control.
|
Possible treatment decisions:
|
Making decisions for someone else can be a difficult and stressful time. A person who makes decisions on behalf of a family member is called a substitute or surrogate decision maker (SDM). If your family member has a legal document naming a person to make decisions for them, then this person is the substitute decision maker (SDM). If this was not determined in advance, the law provides a list of people who may act as the SDM arranged in order of legal priority: often a spouse, a parent of a child, an adult child of a parent, and so on. We are speaking to you as if you are the patient’s SDM. This is an opportunity for you to represent your loved one and help ensure they get the best care possible. We want to help you, the SDM, in making decisions related to your family member’s care plan. You may feel like you need more information to help you in this role.
Your role as a Substitute Decision Maker is to help the ICU team make treatment decisions based on your family member’s previously expressed wishes, values and beliefs. If you do not know what your family member’s wishes are, you, the Substitute Decision Maker, should use your best judgement to make decisions based on how your family member would want to be treated if he or she could decide for him or herself. It is important to resist the natural tendency to make decisions based on how you would want to be treated if you were critically ill. We will ask you to share conversations you may have had with your family member before they became unable to speak for themselves.
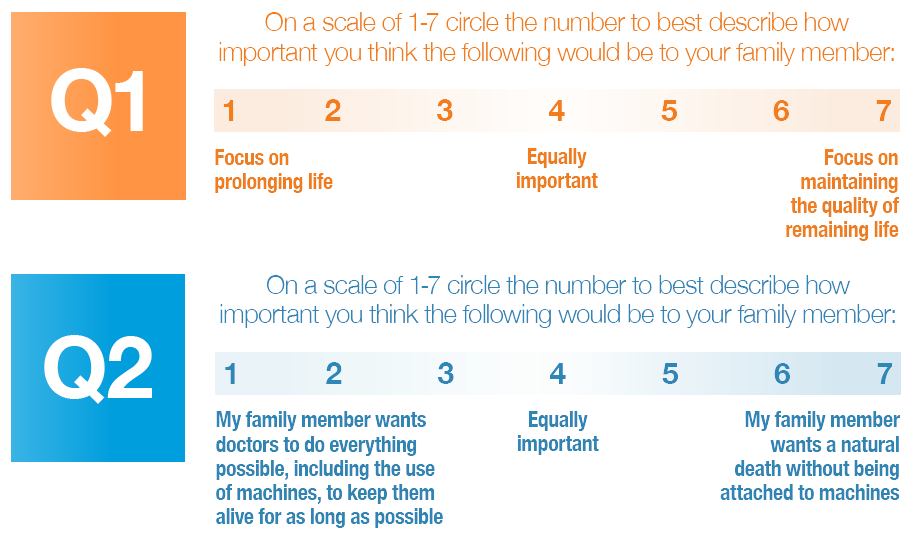
It would be helpful if you could think about the answers to the following values questions.
They will be asked of you again when you go through the ICU questionnaire. Think about your answers to these questions and why you chose those answers. You will be asked to record your answers to these question in the ICU questionnaire.
The doctor in the ICU is a trained expert in treating critically ill people and can provide you with an explanation of the medical problems, a sense of whether your loved one is headed towards recovery or decline, and the overall chances of survival. However, doctors are often uncertain about the chances of recovery or what condition patients will be in if they survive. Nevertheless, they will try to provide you with accurate and honest information about your family member’s chances of recovering and expected long-term quality of life. The doctor may discuss starting new treatments or stopping treatments, such as life support, if they believe they are unhelpful.
Doctors should:
- Ask you about the patient’s life, life style, function and values
- Share with you medical information about the patient’s condition, chances of survival and what kind of function or quality of life they might have
- Ask you to think about the medical information shared with you and ask you to share how you think the patient would have reacted to this information
- Ask you for what medical treatments you think the patient would have preferred
- Propose a treatment plan that is most consistent with the patient’s values, preferences and considerations.
Please Note: If the doctor does not ask for this information, we would encourage you to share it anyway. It is important that the doctor and the clinical team have the same understanding as you do regarding the patient’s function, values, and preferences.
Decision making for a family member who is in the ICU
When you have a loved one in the ICU, the health care team may hold a ‘family conference’ with you to discuss your loved one’s medical condition and decisions that may need to be made.
These videos show conversations between a doctor and a couple with a relative in the ICU. The videos show how you can use the My ICU Guide questionnaire when discussing your loved one’s care.
The first video features a doctor who is familiar with the My ICU Guide website and the second video features a doctor who is not familiar with the website.
People often find themselves overwhelmed with the thought of making a decision for a critically ill family member, particularly when there is so much uncertainty about what is the best decision. It is important to understand that you should never be asked to make a decision alone. Some people do not want to make decisions at all and prefer that the medical team makes the decisions while others prefer to be more involved. As the Substitute Decision Maker, you can also talk with other family members and friends to help with decision-making. In most circumstances, the family and the health care team will work together to make the best decision for the patient. Your main role is to represent the wishes, beliefs and values of the patient. The health care team’s main role is to provide you with information and explore the treatment options for your family member. As a team, you and the healthcare providers can make decisions that balance your family member’s wishes, beliefs and values with the treatment options available. These decisions form the foundation of the care plan moving forward.
It’s important to remember that just because you want something for your family member, it doesn’t mean you will always automatically get it. The medical treatments they will receive depend on their values and preferences, but also their illness, the doctor’s recommendations, and your family member is responding to current treatments.
Despite the best efforts of the ICU staff, sometimes patients are too ill and do not survive. A person dies when their heart stops beating or they are declared brain dead. If the doctors believe the patient is brain dead, they have a set of tests they must follow to confirm this. If the patient has died the next of kin and family members may be approached to discuss organ donation. Knowing the patient’s wishes regarding organ donation can help in making the right decision for your family. Most families who agree to donate one or more of the patient’s organs find it comforting that something good will come from their loss. It may help you to talk to a bereavement counselor at this difficult time. They can offer support and understanding for adults and children. Funeral homes may be a helpful resource in connecting you with consellors and support in the community.